
8 STI Symptoms You Should Never Ignore
Table of contents
- What’s the Difference Between an STI and an STD?
- How Common Are STIs?
- How Often Should You Get Tested?
- What Signs and Symptoms Should I Be Aware Of?
- What Else Can I Do to Prevent an STI?
- Related Content
The various ways we can show intimacy and be sexually active requires us to be aware of our sexual health, both for ourselves and for the people we meet. And while sexual health includes many issues, including consent, family planning (when pregnancy is possible), maximizing pleasure and minimizing pain, it also means doing one’s part in preventing sexually transmitted infections (STIs). While STIs can oftentimes be asymptomatic, there are also many symptoms to be on the lookout for in symptomatic cases.
To help better understand some of the common symptoms associated with STIs and symptoms to be aware of, we spoke to Carl Streed Jr MD MPH — an Assistant Professor of Medicine in the Boston University School of Medicine, who has chaired the American Medical Association Advisory Committee on LGBTQ Issues and served on the board of GLMA: Health Professionals Advancing LGBTQ Equality. In addition to being a primary care clinician, Dr. Streed is the Research Lead for the Center for Transgender Medicine and Surgery at Boston Medical Center and collaborates with researchers, clinicians, and staff to assess and address the health and well-being of transgender and gender diverse individuals.
Here is what Dr. Streed had to say about STIs, STDs, and how to put your sexual health in your own hands:
What’s the Difference Between an STI and an STD?
You’ll see these terms used interchangeably, but there is a subtle difference between sexually transmitted infections (STIs) and sexually transmitted diseases (STDs). Specifically, STIs cause STDs. Common STIs include bacterial vaginosis, chlamydia, gonorrhea, genital herpes, hepatitis, HIV, human papillomavirus (HPV), syphilis, and trichomoniasis, to name a few. You can have any one of these STIs without having an STD; you can be asymptomatic, meaning you have no active disease or symptoms. However, this could mean you can transmit the infection to others. Since many STIs can be asymptomatic, routine testing even when you do not have symptoms is part of routine health care.
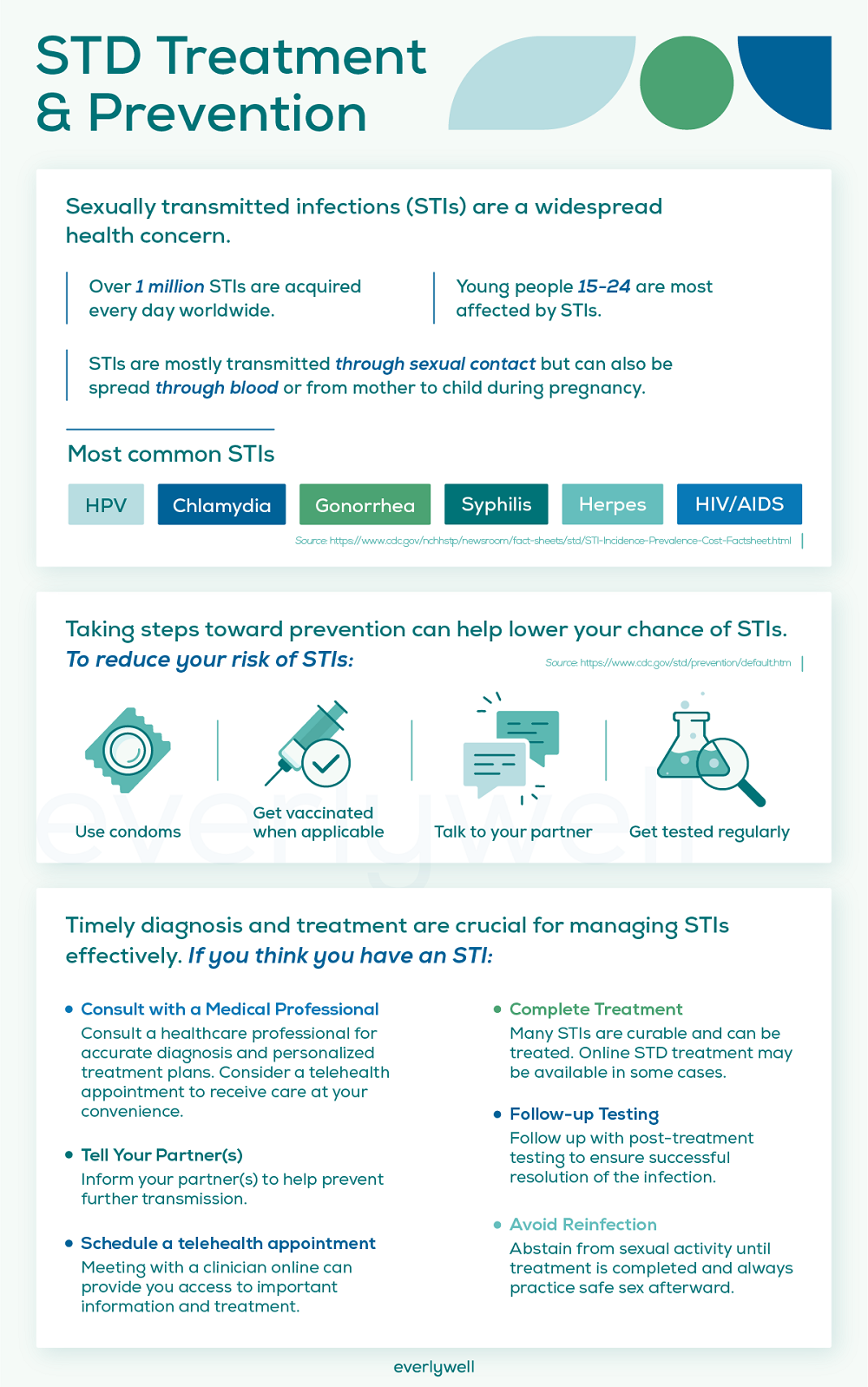
How Common Are STIs?
In the US, 1 in 5 people have a STI with nearly half of all new infections among persons 15 to 24 years of age.[1] One misconception is that STIs are just an issue for younger folks but anyone who is sexually active, at any age, could get an STI. Common STIs, such as chlamydia, can result in few if any symptoms but can pose a risk for transmission; over half of all persons with a chlamydia infection have no symptoms (e.g., no pain, no discharge).
How Often Should You Get Tested?
Given the high likelihood of having an STI even if you have no symptoms, it is important to undergo routine STI screening.[2] Doing so allows you to get treatment and protect yourself and those with whom you’re sexually active. If you’re sexually active, it is recommended that everyone have annual testing for HIV, syphilis, chlamydia, gonorrhea, and trichomoniasis. People who engage in anal intercourse are advised to consider more frequent testing (every 3 to 6 months). Your individual testing schedule depends on how many people you have sex with and what you do when you have sex.
What Signs and Symptoms Should I Be Aware Of?
While many STIs may not cause symptoms, you may want to get tested if you have any of the following issues:
1. Painful urination A burning sensation or severe discomfort when you urinate can be a sign of an infection, such as chlamydia and/or gonorrhea. This can also be associated with the urge to urinate more often. Oftentimes, these symptoms can be confused with a urinary tract infection and not as a result of sexual activity.
2. Pelvic or lower abdominal pain or irritation Lower abdominal pain, particularly in the pelvic region, could be a sign for an STI and warrants getting tested either with a urine test,vaginal/cervical swab, and/or rectal swab.
3. Painful defecation If you engage in anal intercourse (“bottoming”) it is possible to get an STI, like chlamydia or gonorrhea. These can cause pain with defecation.
4. Abnormal anal, urethral, or vaginal discharge Any kind of discharge or “drip” could be a sign of an STI, especially chlamydia and/or gonorrhea.
5. Persistent sore throat If you engage in any oral sex, including cunnilingus, analingus, or fellatio, you could contract an STI of the throat. A persistently sore throat could be a sign of a gonorrhea infection. If you’ve recently performed oral sex and have had negative testing for other common throat infections (e.g., Strep), consider testing for an STI.
6. New bumps or sores If you have a new bump in an area where you’ve had sexual contact (e.g., mouth, labia, penis, anus) it is worth considering testing for an STI. Many STIs can present as a new bump, either painless or painful. Herpes and syphilis are two common STIs that can cause bumps that warrant testing.
7. Blood in urine Chlamydia and gonorrhea infections can cause blood in the urine. Blood in the urine can be as faint as a pale pink or orange and often associated with pain with urination.
8. Blood in stool Just like with pain with defecation, persistent blood in the stool could be a sign of an STI if you engage in anal intercourse (“bottoming”).
What Else Can I Do to Prevent an STI?
In addition to appropriate screening and testing when you have symptoms of an STI, there are additional ways to safeguard your sexual health. Condoms remain the mainstay of preventing STIs, particularly chlamydia, gonorrhea, syphilis, and HIV. However, there are additional layers of protection to prevent STIs.
There are several vaccines worth getting:
Hepatitis: getting vaccinated against Hepatitis A and Hepatitis B can add another layer of protection against liver disease and even some forms of liver cancer.[3]
HPV: the HPV vaccine has reduced the risk infection, genital warts, and cancers by upwards of 88%[4]
Meningococcal: there are some bacterial STIs that can cause severe infection, like meningitis Thankfully, there are two vaccines available against a common cause of meningitis.[5]
The addition of Pre-Exposure Prophylaxis (PrEP) against HIV has been a game changer to reduce the number of new HIV infections. If you’re concerned about HIV infection, consider learning more about HIV PrEP and having additional peace of mind.
Making regular testing part of your health routine not only prevents the spreading of infection to the people you meet — it allows for more pleasurable sexual experiences with the least discomfort.
Everlywell's Virtual Care Visits provide a convenient way to manage sexual health, allowing for STD telehealth consultations within 2 hours. This service extends to include bacterial vaginosis online treatment and genital herpes online treatment, ensuring comprehensive care options are accessible from the privacy of your home. With the right tests and prescriptions, Everlywell aims to offer timely and effective recommendations for those in need.
You can also opt for sexual health testing year-round through the Everlywell+ health tests membership, giving you easy access to a wide of variety of sexual wellness testing options.
Related Content
STDs in Older Adults: Everything You Need to Know as You Age
STD vs. Yeast Infection: 4 Differences in Symptoms
References
- Sexually Transmitted Infections Prevalence, Incidence, and Cost Estimates in the United States. Centers for Disease Control and Prevention. Sexually Transmitted Diseases (STDs). https://www.cdc.gov/std/statistics/prevalence-2020-at-a-glance.htm. Accessed February 8, 2022.
- Screening Recommendations and Considerations Referenced in Treatment Guidelines and Original Sources. Sexually Transmitted Infections Treatment Guidelines, 2021. Centers for Disease Control and Prevention. https://www.cdc.gov/std/treatment-guidelines/screening-recommendations.htm. Accessed February 8, 2022.
- Hepatitis B Questions and Answers for the Public. Viral Hepatitis. Centers for Disease Control and Prevention. https://www.cdc.gov/hepatitis/hbv/bfaq.htm#bFAQd01. Accessed February 8, 2022.
- Reasons to Get HPV Vaccine. Human Papillomavirus. Centers for Disease Control and Prevention. https://www.cdc.gov/hpv/parents/vaccine/six-reasons.html. Accessed February 8, 2022.
- Meningococcal Vaccination: What Everyone Should Know. Vaccines and Preventable Diseases. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/vpd/mening/public/index.html. Accessed February 8, 2022.