Is hypertension cardiovascular disease?
Written on February 27, 2023 by Theresa Vuskovich, DMD. To give you technically accurate, evidence-based information, content published on the Everlywell blog is reviewed by credentialed professionals with expertise in medical and bioscience fields.
Table of contents
- What is hypertension?
- Hypertension can have several causes
- How do you know if you have hypertension?
- What is the best treatment for hypertension?
- Virtual care visits via Everlywell
- Related content
You may be wondering, “Is hypertension a cardiovascular disease?” Hypertension (high blood pressure) is not a cardiovascular disease, but high blood pressure is the leading cause of cardiovascular disease [1-3]. Cardiovascular or heart disease remains the primary cause of death in the United States [1,2]. Understanding hypertension and heart disease is essential for staying healthy.
What is hypertension?
Hypertension occurs when your blood pressure is consistently high, which stresses your heart and other organs [1,2]. High blood pressure means you consistently have a blood pressure reading of 130/80 mm Hg or higher [1,2]. The first number is called your systolic blood pressure and represents the pressure your blood exerts on your artery walls. The second number is your diastolic blood pressure which represents blood pressure against artery walls while your heart rests.
As your blood pressure rises, your risk of heart disease increases. There are three levels of hypertension [1-3]. Here are the three categories of hypertension [1-3]:
- Stage 1 hypertension: systolic 130–139 mmHg or diastolic 80–89 mmHg
- Stage 2 hypertension: systolic 140-180 mmHg or diastolic 90-120 mmHg
- Stage 3 hypertension: systolic over 180 mmHg or diastolic over 120 mmHg
A healthcare provider must confirm a hypertension diagnosis [3]. You need a consistently high blood pressure reading to get a diagnosis. When you're stressed or exercising, your blood pressure may rise, but it should quickly return to a healthy level.
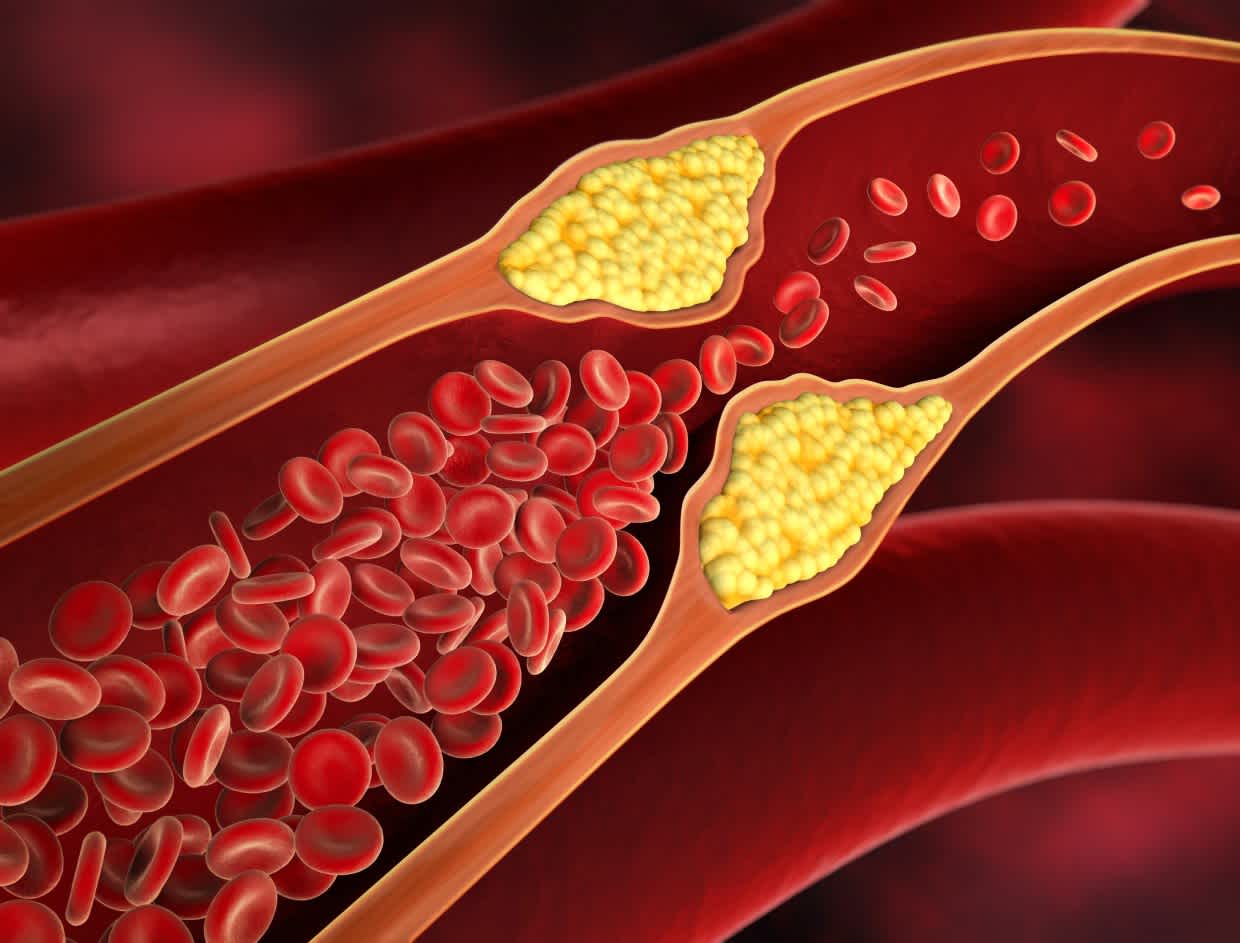
High blood pressure can cause heart disease due to the stress it puts on your heart [1]. Hypertension damages the lining of your blood vessels, causing plaque buildup and making your heart work harder [1-3]. Over time, your heart may weaken [1].
Hypertension can have several causes
High blood pressure can occur due to primary or secondary causes. Primary hypertension typically results from modifiable lifestyle factors, but the exact cause is often unknown [3,4]. On the other hand, secondary hypertension is caused by a medical condition or medication(s) [3,4]. Medical conditions such as kidney disease can cause hypertension, as can drugs such as nonsteroidal anti-inflammatory drugs (NSAIDs) [2].
Primary hypertension is the most common type of hypertension [3,4]. Primary hypertension is caused by [3,4]:
- Eating or drinking too much sodium
- Drinking too much caffeine
- Being overweight
- Experiencing psychosocial stress
- Drinking too much alcohol
- Having a sedentary lifestyle
- Having sleeping problems such as insomnia or obstructive sleep apnea (OSA)
Most primary hypertension risk factors are modifiable, meaning you can change your lifestyle to reduce your risk [1-5]. Some people do have a genetic predisposition to developing hypertension [3]. Genetics are thought to account for between 35% and 50% of your risk for developing hypertension [3].
An example of a genetic disease associated with hypertension is familial hypercholesterolemia (FH) [6]. FH is a genetic disease causing elevated cholesterol levels resulting in hypertension [6].
However, for most people, high blood pressure is preventable [3]. The best ways to prevent hypertension include [7,8]:
- Following a plant-based and Mediterranean diet rich in fruits, nuts, vegetables, legumes, and lean protein (ideally fish)
- Reducing your sodium, red meat, and sugar-sweetened beverages (SSB intake)
- Engaging in at least 150 minutes of moderate or 75 minutes of vigorous activity per week
- Remaining active throughout the day
How do you know if you have hypertension?
Hypertension is known as the "silent killer" due to its lack of symptoms [11]. As a result, it is important to check your blood pressure often and see your healthcare provider regularly.
Symptoms usually appear only after someone has had high blood pressure for a long time. You may have hypertension if you frequently experience the following symptoms [4]:
- Having blurred vision
- Experiencing shortness of breath and chest pain
- Feeling dizzy, lightheaded, or tired
- Having frequent nosebleeds or severe headaches
You can also determine if you are at a greater risk of developing hypertension by measuring your cholesterol and C-reactive protein levels. You can gain insight into your heart health with Everlywell's heart health test.
What is the best treatment for hypertension?
The best treatment for hypertension is making your lifestyle healthier. If lifestyle modifications do not improve your blood pressure, your healthcare provider may prescribe medications. Treatment for hypertension usually requires combination therapy, which involves taking two or more drugs together [2].
You and your healthcare provider will discuss the best medication options for you. First-line treatment for hypertension usually involves three types of medication [2, 4, 9-13]:
1. Angiotensin-Converting Enzyme Inhibitors (ACE inhibitors or ACEIs) or Angiotensin Receptor Blockers (ARBs): ACE inhibitors lower blood pressure by decreasing angiotensin production. ARBs allow the heart to pump blood more efficiently by relaxing blood vessels. ACE inhibitors are preferred over ARBs. However, if you are taking an ACE and experiencing side effects, your healthcare provider may prescribe an ARB. ACE inhibitors and ARBs are never prescribed together.
Common ACE inhibitors include:
- Lisinopril (Prinivil, Zestril)
- Enalapril (Vasotec)
- Benazepril (Lotensin)
Common ARBs include:
- Losartan (Cozaar)
- Telmisartan (Micardis)
- Valsartan (Diovan)
2. Calcium Channel Blockers (CCBs): CCBs decrease blood pressure by relaxing blood vessels, making it easier for the heart to pump blood.
Common CCBs include:
- Amlodipine (Norvasc)
- Nifedipine (Procardia)
- Diltiazem (Cardizem)
3. Thiazide Diuretic: Diuretics are also called "water pills" and function in the kidneys to remove excess salt and water.
Common diuretics include:
- Chlorthalidone
- Hydrochlorothiazide (Microzide)
- Metolazone
If you are taking medication to treat hypertension, your target blood pressure is 130/80 mm Hg [7]. If your prescription is causing side effects or not controlling your blood pressure, your healthcare provider may adjust the dosage or medication. You and your healthcare provider can work together to ensure the medications are making you feel your best.
Virtual care visits via Everlywell
You can speak with a healthcare provider through Everlywell. During a 30-minute video appointment, you can discuss your health goals with a nurse practitioner. Visit our Virtual Care Visits page to make an appointment. Additionally, you may be interested in checking in on your heart health with the Heart Health Test, which measures total cholesterol, HDL, calculated LDL, triglycerides, hs-CRP and HbA1c.
Related content
Heart disease and stroke: what you need to know
How breakfast is important for heart disease
What causes coronary heart disease?
How long do heart attacks last?
Do you need an AED when performing CPR?
References
- Heart disease and stroke. Centers for Disease Control and Prevention. URL. Published September 8, 2022. Accessed February 23, 2023.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2018;71(6):e13-e115. doi:10.1161/HYP.0000000000000065. URL
- Oparil S, Acelajado MC, Bakris GL, et al. Hypertension. Nat Rev Dis Primers. 2018;4:18014. Published 2018 Mar 22. doi:10.1038/nrdp.2018.14. URL
- What to know about essential hypertension (primary hypertension). Cleveland Clinic. URL. Accessed February 23, 2023.
- High blood pressure symptoms and causes. Centers for Disease Control and Prevention. URL. Published December 6, 2022. Accessed February 22, 2023.
- Bianconi V, Banach M, Pirro M, International Lipid Expert Panel (ILEP). Why patients with familial hypercholesterolemia are at high cardiovascular risk? Beyond LDL-C levels. Trends Cardiovasc Med. 2021;31(4):205-215. doi:10.1016/j.tcm.2020.03.004. URL
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140(11). doi:10.1161/cir.0000000000000678. URL
- Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279-1290. URL
- High blood pressure–understanding the silent killer. U.S. Food and Drug Administration. URL. Accessed February 23, 2023.
- Frank J. Managing hypertension using combination therapy. Am Fam Physician. 2008;77(9):1279-1286. URL. Accessed February 22, 2023.
- Prevent high blood pressure. Centers for Disease Control and Prevention. URL. Published October 18, 2022. Accessed February 22, 2023.
- Tazkarji B, Ganeshamoorthy A, Auten B. Angiotensin-converting enzyme inhibitors vs. Angiotensin receptor blockers. Am Fam Physician. 2015;91(3):193-194. URL. Accessed February 23, 2023.
- Choice of drug therapy in primary (essential) hypertension. UpToDate. Uptodate.com. URL. Accessed February 23, 2023.