Why the new HPV test might be better than the Pap smear at detecting cervical cancer risk in women
Table of contents
- The HPV and cervical cancer link
- New HPV test better at detecting cervical cancer risk than Pap smear?
- What if you test positive for high-risk HPV?
- Related content
It’s happening somewhere right now: a woman is on her way to the gynecologist for a Pap smear (or Pap test). As you may know, a Pap smear – or a “pap” – screens for cervical cancer. If signs of cervical cancer are detected early enough, there’s a good chance that prompt medical intervention can defeat the cancer (or precancerous cells). However, as anyone who’s gotten a Pap smear knows, this test isn’t exactly the most comfortable of experiences. Still, many women regularly get Pap tests to thwart the risk of cervical cancer. And, until recently, no other screening methods for cervical cancer existed which were as accurate as the pap.
But that situation could very well be changing. Exciting new research suggests that a much less invasive approach – the HPV test – may even more accurately screen for cervical cancer risk. And, what’s more, sample collection for the HPV test can be done at home by yourself – a major difference between this test and the traditional Pap smear.
But why can this groundbreaking new test clue you in on your cervical cancer risk? It’s because there’s an unequivocal link between HPV – a type of virus – and cervical cancer.
The HPV and cervical cancer link
HPV is a type of virus that spreads through sexual contact. So, strictly speaking, anyone who is sexually active – women and men alike – can get an HPV infection. (HPV stands for “human papillomavirus.”)
However, not all HPV infections carry the same health implications because there are many different strains of the virus. In fact, there are close to 200 different HPV strains!
Broadly speaking, though, HPV strains can be divided into two main camps: low-risk and high-risk types – or “genotypes” in the biologist’s vernacular.
“Low risk and high risk of what?” you may be wondering.
And the answer? Cervical cancer.
Low-risk HPV types don’t lead to cancer. However, they can cause genital warts – a non-life-threatening infection that’s both quite common and quite treatable. It’s estimated that roughly 1 out every 100 sexually active adults in the United States have genital warts.
But now let’s shift our focus to high-risk HPV types – those microscopic invaders that can inflict heavy damage on the body, and particularly the cervix, resulting in cervical cancer. And cervical cancer isn’t in the same league as genital warts – which are, in comparison, just a minor nuisance. Cervical cancer can be deadly – particularly when it goes undetected and untreated for a while.
Just how deadly is cervical cancer?
Every year, about 4,000 women in the United States pass away due to cervical cancer – and about 12,000 women are diagnosed with the disease. Those numbers seem somewhat large considering that screening and treatment protocols are available in clinics throughout every state in the nation.
And at fault for practically all cases of cervical cancer are the high-risk HPV types – particularly the types designated by the numbers 16 and 18 (which cause about 70% of cervical cancer cases). High-risk HPV types, then, are very closely linked with cervical cancer – in fact, high-risk HPV is associated with 99% of all cervical cancer cases, prompting one researcher to comment, “The associations observed between the infection by [high-risk] HPV and cervical cancer are among the highest ever identified in human cancerology.”
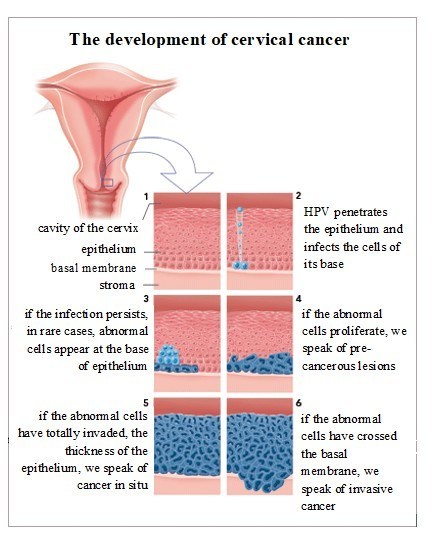
So if there was a test that could detect these high-risk HPV types in the body, then it could be used to screen women at risk for cervical cancer – and with a high degree of accuracy.
That is the idea behind the HPV test (which you can use at home), which screens for cervical cancer risk by identifying exactly what high-risk HPV types – if any – you have. For example, if an HPV test indicates the presence of HPV 16 or 18, then there’s a much greater risk of cervical cancer developing compared to other HPV types if left unchecked and untreated. Appropriate treatment could then be promptly done, drastically minimizing the chances of cervical cancer.
New HPV test better at detecting cervical cancer risk than Pap smear?
Recent research points to the strong possibility that the HPV test is better at detecting cervical cancer risk than the traditional, not-all-that-pleasant Pap test. The HPV test can also pick up on indicators of cervical cancer risk even if a Pap test fails to do so.
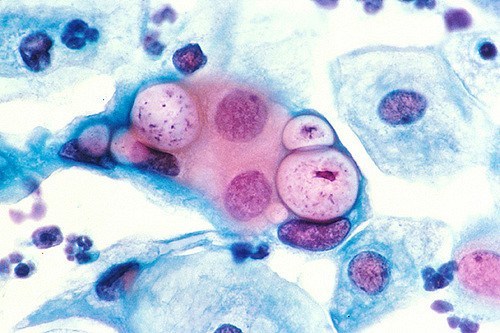
Why might the HPV test be more accurate than the Pap smear? For starters, the Pap smear process is not infallible – accuracy of results greatly rely on a cytologist’s visual interpretation of cervical cells. And where one finds interpretations based on human senses – like sight – one will invariably also find human error. Such is the case for the Pap smear, and it is because of such errors that one cytopathologist noted that “in the real world, the goal of completely conquering cervical cancer is probably impossible to achieve through Pap smear screening.”
Cytologists frequently analyze dozens of Pap smears per day – tedious work that’s been described as “boring” and extraordinarily monotonous. So the occasional fatigue and inattention that can set in may cause the technician to overlook less obvious signs of cancer in the smear.
This is not to say that the Pap test is not – and has not been – effective. On the contrary, actually, it’s one modern medicine’s great triumphs: the most successful test ever devised in the 20th century for preventing cancer. Despite this, women in the United States are still dying from cervical cancer – so it’s clearly good news that a possibly more accurate test is here that can reliably screen for cervical cancer risk.
There are several reasons why the HPV test may be more accurate than the Pap test, but one of the major ones is that HPV test results are less ambiguous and more clear-cut. That’s because the HPV test determines the DNA sequence of any HPVs found in the smear. This DNA sequence provides powerful molecular data on cervical cancer risk (as different HPV types are associated with varying degrees of risk). So, with the HPV test, assessing results simply involves taking a look at straightforward molecular information – instead of peering into a microscope and trying to find sometimes subtle hints of cancerous changes in cervical cells.
What if you test positive for high-risk HPV?
If you test positive for high-risk HPV, this doesn’t mean you’ll absolutely get cervical cancer. That’s because – in many cases – the body can actually clear away an HPV infection on its own. In fact, a very large number of sexually active people get high-risk HPV infections in their 20s – but the body can usually mount a successful defense and defeat the virus before any cancer develops. However, if high-risk HPV persists in the body for years and years, then there’s a much greater risk that the HPV isn’t going away anytime soon – and might trigger the onset cervical changes that can lead to cervical cancer. For that reason, HPV testing is especially vital for women who are aged 30+. With Everlywell, you can take an HPV test at home.